This was an independent study project I did during my Bioethics program in 2016. It will need revision to address epidemics like COVID-19.
Policy: Adult Ventilator Allocation PDF
Paper: Implementing a Pandemic Influenza Ventilator Allocation Plan PDF
PURPOSE: To outline the procedure for allocating adult mechanical ventilators during a pandemic and a statewide ventilator shortage.
POLICY STATEMENTS: When New York State Department of Health has declared a statewide ventilator shortage, [Hospital/System] will allocate mechanical ventilators using the process outlined in this document.
A limitation in resources shifts the priority of [hospital/system] ministry from individual patients to the overall population. In the event of pandemic influenza where the demand for mechanical ventilation exceeds the ability to supply mechanical ventilation (due to inadequate supply or inadequate ability to provide staff), [hospital/system] will allocate mechanical ventilation equipment in a just, ethical manner and in accord with New York State guidelines on ventilator allocation. While it is impossible to predict every scenario, this policy will assist physicians with triaging which adult patients should receive mechanical ventilation in a just and equitable manner and will ensure that ventilator allocation decisions are made in a consistent manner between physicians.
SCOPE OF AUTHORITY / COMPETENCY: Physicians, physician assistants, nurse practitioners, adult critical care nurse managers, respiratory therapy managers.
PROCEDURE
Triage committee: Triage decisions will be made by a triage committee composed of a physician, critical care nurse manager, and respiratory therapy manager. This committee will have access to information about staffing, bed availability, and ventilator availability. The committee will be provided relevant clinical data as outlined below to make objective decisions about ventilator allocation. This committee removes triage responsibilities from the bedside physician to allow them to focus on patient care.
Triage of patients will follow the criteria below, adapted from NYS Task Force on Life and the Law’s Ventilator Allocation Guidelines (2015). This procedure applies not only to new critical care admissions but will also be applied to all patients currently on mechanical ventilation at the time the Department of Health declares a statewide shortage of ventilators and [hospital/system] acute care hospitals are operating at surge capacity.
Exclusion Criteria: Patients with medical conditions that result in immediate or near-immediate mortality even with aggressive therapy will be excluded from receiving mechanical ventilation:
• Cardiac arrest: unwitnessed arrest, recurrent arrest without hemodynamic stability, arrest unresponsive to standard interventions and measures.
• Trauma-related arrest.
• Irreversible age-specific hypotension unresponsive to fluid resuscitation and vasopressor therapy
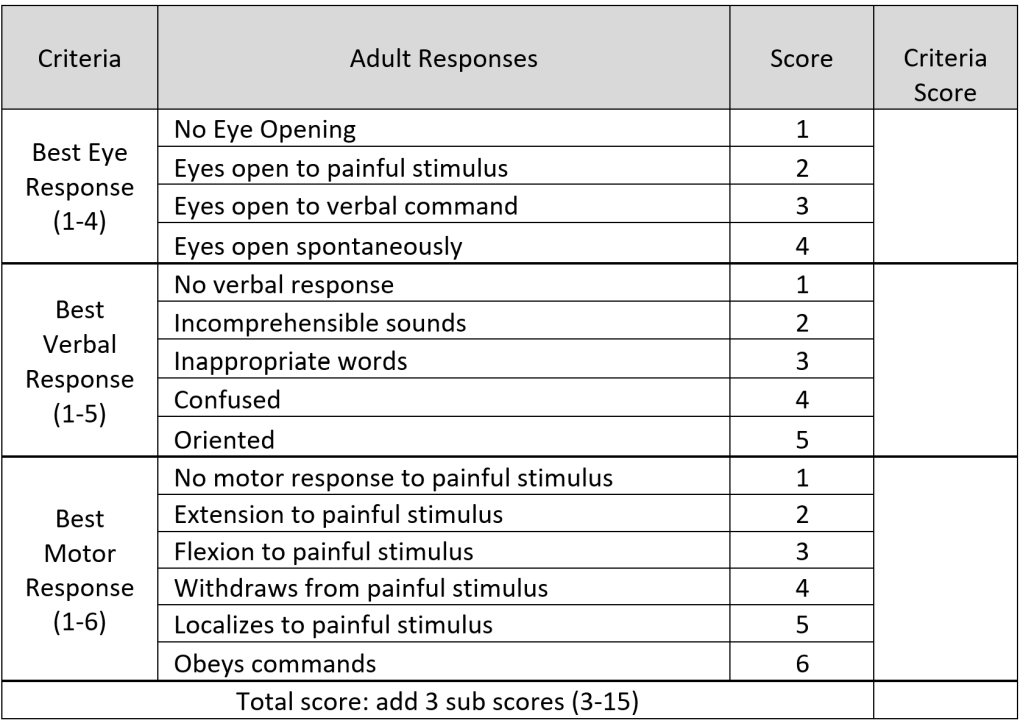
• Traumatic brain injury with no motor response to painful stimulus (i.e., best motor response = 1 on Glasgow Coma Scale).
• Severe burns: where predicted survival ≤ 10% even with unlimited aggressive therapy. (See Appendix: Burn Triage table, expectant category)
• Any other conditions resulting in immediate or near-immediate mortality even with aggressive therapy.
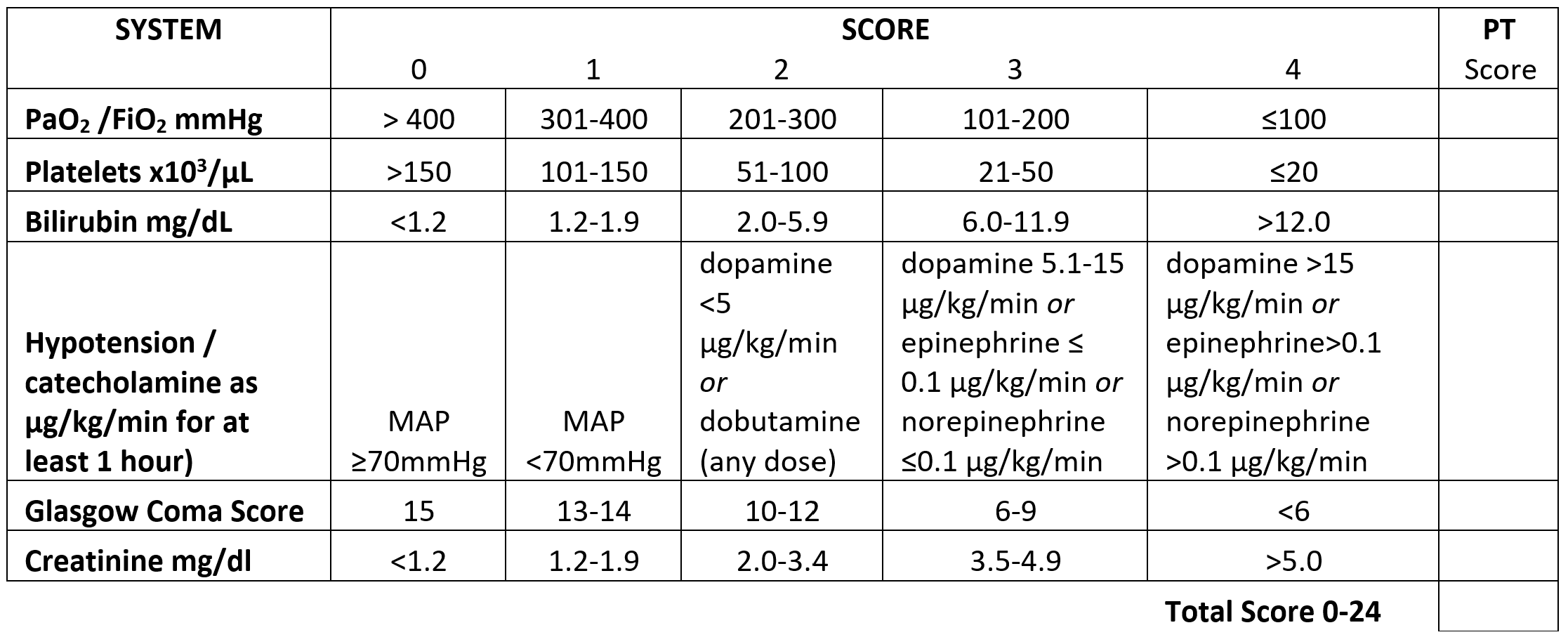
Mortality Risk Assessment: For patients who aren’t excluded based on the above criteria, a mortality risk assessment will be made using the Sequential Organ Failure Score (SOFA). (Ferreira 2001, p1754) This assessment is performed when the patient is initially triaged and again at 48 hours and 120 hours after the initial assessment.
Ferreira FL, Bota DP, Bross A, Mélot C, Vincent J. Serial Evaluation of the SOFA Score to Predict Outcome in Critically Ill Patients. JAMA. 2001;286(14):1754-1758. doi:10.1001/jama.286.14.1754
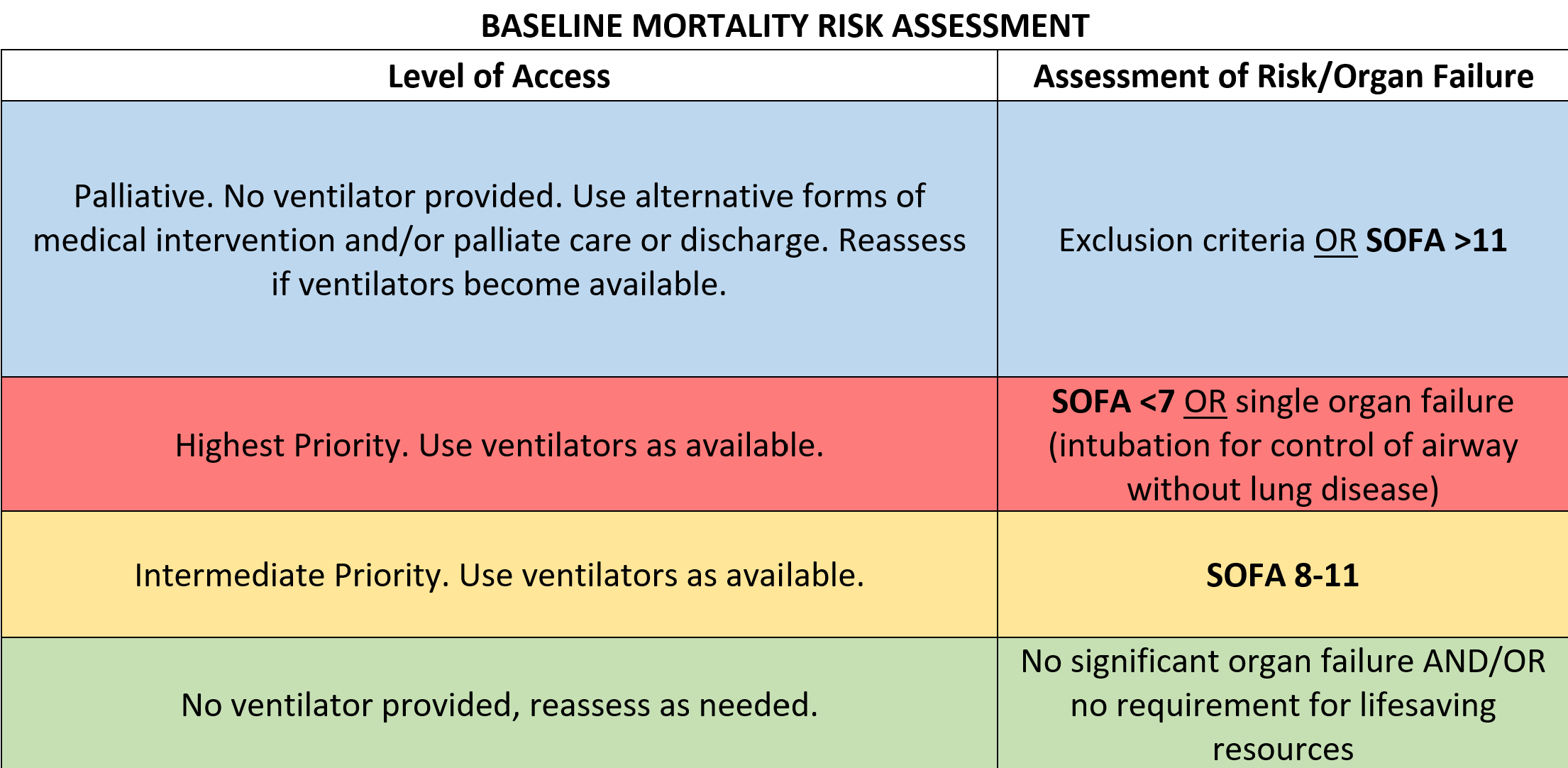
After reviewing exclusion criteria and completing the mortality risk assessment, patients will be triaged to palliative care, high priority, intermediate priority, or low priority.
Baseline Assessment: Based on each patient’s initial mortality risk assessment, they will be categorized as follows. This baseline mortality risk assessment and the disposition of the patient (excluded from mechanical ventilation or initiation of a trial of mechanical ventilation implemented) will be recorded on a ventilator allocation flowsheet.
 New York State Task Force on Life and the Law, New York State Health Department. (2015) Ventilator Allocation Guidelines, p 59
New York State Task Force on Life and the Law, New York State Health Department. (2015) Ventilator Allocation Guidelines, p 59
 New York State Task Force on Life and the Law, New York State Health Department. (2015) Ventilator Allocation Guidelines, p 66.
New York State Task Force on Life and the Law, New York State Health Department. (2015) Ventilator Allocation Guidelines, p 66.
Levels of Access
- Palliative Care (Blue): These are patients with a high risk of mortality. They are not admitted to critical care beds and palliative care should be provided to relieve physical discomfort as well as psychological and spiritual support. A DNR order should be written and appropriate supportive care provided. For patients on mechanical ventilation whose status has deteriorated or failed to improve, they should be removed from mechanical ventilation and transferred out of critical care. When it is determined that a patient should receive palliative care, the rational for this decision should be clearly documented.
- High Priority (Red): High priority patients have a moderate risk of mortality. They are the most likely to recover with ventilator support and likely to not recover without it. These patients should receive a trial of mechanical ventilation when ventilators are available.
- Intermediate Priority (Yellow): These are patients who are very sick on initial assessment and may or may not benefit from mechanical ventilation or who are showing minimal improvement on subsequent assessments. Patients in this intermediate category may receive a trial of ventilator support only after all patients in the high priority group have received support.
- Low Priority (Green): These are patients who will likely survive without ventilator therapy. Other modes of respiratory support such as non-invasive ventilation and oxygen therapy may be used as needed
High priority patients are to be allocated ventilator patients first. If there are more high priority patients than available ventilators, a randomization process should be used to allocate the ventilators. Once all high priory patients have received ventilators, then remaining ventilators may be allocated to intermediate priority patients in a similar manner. If any ventilators remain, any patients that may have otherwise received only palliative care or alternative therapy may be considered for mechanical ventilation. (See also: Removing patients from mechanical ventilation)
If a patient needs mechanical ventilation and no ventilator is available, alternative therapies and/or palliative care should be used to optimize support until a ventilator becomes available.
Time Trials: Once a mechanical ventilation trial is initiated, a mortality risk assessment is repeated at 48 hours and 120 hours. At each interval, each patient is reassessed and triaged according to the following criteria. “Time trials are necessary because they provide as many patients as possible with sufficient opportunity to benefit from ventilator therapy. The use of time trials ensures uniform official assessments and provides valuable information about the status and real-time availability of ventilators.” (NYS Taskforce, 14)
Between the baseline, 48 hour, and 120 hour assessments, patients receiving mechanical ventilation will continue to be monitored as per standard protocols. “Although additional clinical assessments may be performed, the official SOFA assessments only occur after 48 and 120 hours of ventilator therapy. No formal triage decision or action may be taken until a patient’s official assessment.” (NYS Taskforce, 15) However, if between the scheduled assessments, a patient is identified as meeting the exclusion criteria, palliative care should be considered and mechanical ventilation should be discontinued if an eligible patient of high or intermediate priority is waiting for a ventilator.
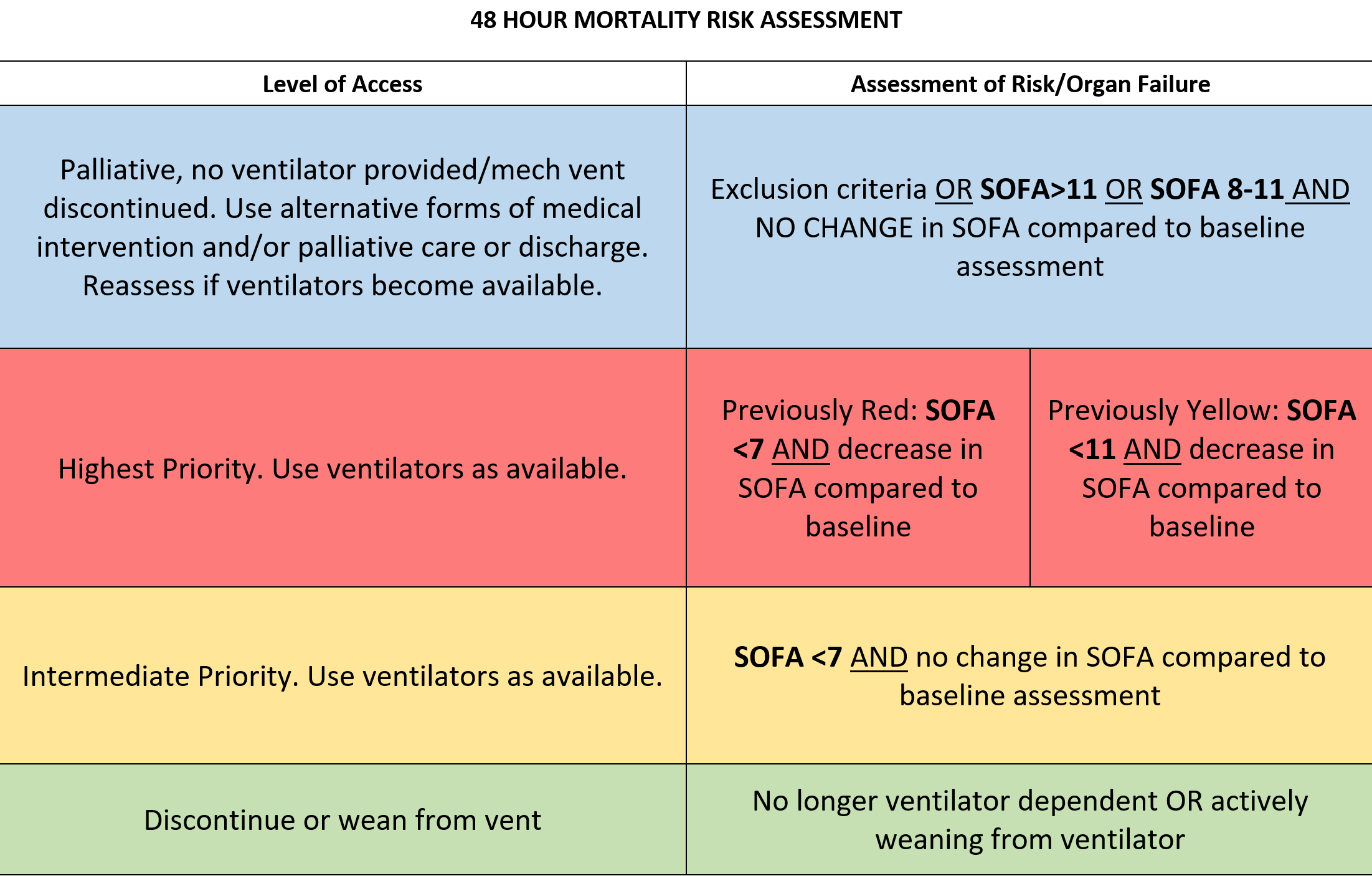 New York State Task Force on Life and the Law, New York State Health Department. (2015) Ventilator Allocation Guidelines, p 64.
New York State Task Force on Life and the Law, New York State Health Department. (2015) Ventilator Allocation Guidelines, p 64.
Beyond 120 hours: Any patient who is continued on mechanical ventilation at the 120 hour mortality risk assessment will be reevaluated every 48 hours by the triage committee using the SOFA criteria. The decision to continue mechanical ventilation at each assessment should be based on SOFA criteria with consideration of clinical improvement or deterioration, the underlying diagnosis and its known progression, current status of pandemic and available resources, and alternatives for care (treatment options, transfer to another facility).
Removing patients from mechanical ventilation: A patient will be continued on mechanical ventilation until the 48 or 120-hour assessment except in the case of a patient meeting exclusion criteria between assessments while a high or intermediate priority patient is waiting for a vent. If at a 48-hour or 120-hour assessment there is a high priority patient waiting to begin mechanical ventilation, it will be necessary to remove from the ventilator a patient who meets the criteria for palliative care. If there is more than one who meets the criteria for palliative care at that point, a randomization process should be used to select which patient will be removed from ventilation. If there are no patients who meet the palliative care criteria but there is a patient receiving ventilation who meets the intermediate priority criteria, the same process would apply to allow the high priority patient access to mechanical ventilation. If all the patients currently receiving mechanical ventilation are in the high priority category, none of the patients would be removed from mechanical ventilation and the incoming patient would be provided supportive alternative therapies until a ventilator became available.
Appeals and Reviews: A review committee, consisting of a physician, adult critical care nursing or respiratory therapy manager, and ethics committee member should meet daily to review any decisions to withhold or withdraw ventilator support and verify compliance with this policy. This process will enable rapid identification of needed adaptations of the policy as the pandemic evolves and new information becomes available. None of these committee members should be on the triage committee currently responsible for determining the patient’s course of therapy nor should the physician on the committee be the physician providing bedside care.
If there is a perceived procedural or technical injustice (such as if a decision is made without considering all relevant data), a real-time appeal may be requested of this same committee.
Alternative Interventions: When there are no ventilators available for high and intermediate priority patients, the best available respiratory support should be provided using oxygen therapy (including high-flow) and non-invasive positive pressure ventilation. The use of manual ventilation by ambu-bag is discouraged in this situation due to the level of staffing required for such support (especially when the length of time this support would need to be provided is unknown) and the increased risk of virus transmission. All patients who are not candidates for mechanical ventilation based on exclusion criteria or SOFA score should be provided with palliative care or hospice support.
Documentation: All triage baseline, 48h and 120h assessments will be documented using the Pandemic Influenza Ventilator Allocation Worksheets.
APPENDICES
Determining Traumatic Brain Injury – Glasgow Coma Scale
Burn Triage

(Taylor, S., Jeng, J., Saffle, J. R., Sen, S., Greenhalgh, D. G., & Palmieri, T. L. (2014, January/February). Redefining the Outcomes to Resources Ratio for Burn Patient Triage in a Mass Casualty. Journal of Burn Care & Research. 35(1), 41-45. doi:10.1097/bcr.0000000000000034 )
REFERENCES
Ferreira, F. L., Bota, D. P., Bross, A., Melot, C., & Vincent, J. (2001). Serial Evaluation of the SOFA Score to Predict Outcome in Critically Ill Patients. JAMA, 286(14), 1754-1758. doi:10.1001/jama.286.14.1754
New York State Task Force on Life and the Law, New York State Health Department. (2015) Ventilator Allocation Guidelines. Retrieved from: https://www.health.ny.gov/diseases/communicable/influenza/pandemic/ventilators/docs/ventilator_guidelines.pdf